【不孕症】患者在中草藥治療後成功分娩 產婦高齡,卵巢儲備嚴重減少:A 案例報告|沈曉雄醫學博士
06/17/2024 沈氏中醫婦科─沈曉雄醫學博士‧教授
A B S T R A C T
The fecundity of women decreases significantly beginning approximately at age 35 and decreases more rapidly after age 40. Age affects not only the size of the oocyte pool but also the quality of germ cells. Despite the continuous advancement of assisted reproductive technology, infertility remains a challenge for women of advanced maternal age. Here, we present a case of a woman in her forties who had two successful live births after treatment with Traditional Chinese Medicine. At her initial visit (at age 43), the patient presented with a short menstrual cycle and signs of a diminished ovarian reserve (FSH: 26.2 mIU/mL; AMH: 0.23 ng/mL). Three years after her first delivery (at age 47), the patient showed signs of further diminished ovarian reserve (FSH: 27.1 mIU/mL; AMH: 0.07 ng/mL). Notably, after five months of Chinese herbal medicine treatment, she achieved another successful pregnancy, and resulted in a live birth. This case demonstrates that Chinese herbal medicine can have a positive clinical impact on improving hormonal balance and fecundity. Further research is needed to investigate the pharmacokinetics of Chinese herbal medicine in improving fecundity for women of advanced maternal age.
1.Introduction
Advanced maternal age (AMA) is associated with a rapid decline in the production of high-quality oocytes and leads to reduced fertility rates for women over 35 [1]. Despite the continuous advancement of assisted reproductive technology (ART), infertility remains a challenge for women of AMA. Even with in vitro fertilization (IVF), live birth rates in women over 40 remains low [2,3]. Today, there are no optimal treatment options available to counteract age-related infertility, apart from using egg donation [4,5]. Meanwhile, traditional Chinese medicine (TCM) has been used to treat gynecological diseases for more than 2500 years. Zhang Zhongjing (150–219 A.D.), a famous TCM physician and herbologist, dedicated special chapters on gynecological diseases in Essential Prescriptions of the Golden Coffer (Jingui Yaolue) [6]. In recent years, acupuncture and herbal medicine have become more prevalent among women with infertility. More patients are now using acupuncture and herbal medicine to increase their fecundity rates before considering ART or after ART failed [7,8]. Here we present and discuss a case of a patient of AMA with severe diminished ovarian reserve (DOR) who had two healthy pregnancies following treatment with TCM.
2.Case presentation
A 43 year-old female initially visited our clinic on August 20, 2015. The patient complained about not being able to get pregnant after trying with her husband for two years.
Her menarche occurred at age 12. Thereafter, her menstrual cycles were 28–30 days without dysmenorrhea. Since 2014, her menstrual cycles were shortened to 25–27 days, and the menstrual flow was me- dium. The patient had one planned termination of her 6 weeks preg- nancy in 2004. Her last menstrual period (LMP) was on July 24, 2015. The patient took laboratory tests on September 20, 2015, and May 6, 2016. Her serum specimens were collected on menstrual cycle day 3.
The laboratory test results are listed in Table 1. On both days, FSH/LH >
3.Hysterosalpingography (HSG) result from September 25, 2015, was normal. Her husband’s semen analysis values were within the normal range of the laboratory references.
She had previously consulted with two reproductive clinics, she was diagnosed with secondary infertility, severe diminished ovarian reserve. Both clinic had advised her to do IVF, one of them suggested an IVF with donated eggs. However, she wanted to try natural remedies before considering ART. Her basal body temperature (BBT) showed short
E-mail address: xiaoxiongshen@yahoo.com.
https://doi.org/10.1016/j.repbre.2023.12.007
Received 4 November 2023; Received in revised form 17 December 2023; Accepted 20 December 2023
2667-0712/© 2023 The Authors. Publishing services by Elsevier B.V. on behalf of KeAi Communications Co. Ltd. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Table 1
The patient’s laboratory test results. Her serum specimens were collected on day 2 of menstrual cycle.
Sep. 20, May 6, Reference Range
2015 2016
basal FSH 26.20 24.20 Follicular phase: 2.5–10.2 mIU/mL
Postmenopausal: 23.0–116.3 mIU/mL
basal LH 8.20 7.80 Follicular phase: 4.9–12.5 mIU/mL
Postmenopausal: 40.0–54.7 mIU/mL
AMH 0.23 0.63 40–49 yrs <4.50>49 yrs < 0.45. ng/mL
basal 35 45.6 Follicular phase: 19–144 pg/mL
Estradiol
menstrual cycles of 25 days with a slow slope of luteal phase tempera- ture rise and down shift during the first month of treatment (Fig. 1).
We developed a treatment plan to help patients improve ovulation function and luteal function using Chinese herbal formula, named “Fu Kun Tang (Decoction)”. The ingredients are as follows: Rehmanniae Radix preparate (Shu Di Huang) 15 g, Ligustri lucidi Fructus (Nu Zhen Zi)12 g, Corni Fructus (Shan Zhu Yu) 20 g, Cuscutae Semen (Tu Su Zi) 15 g, Cistanches Herba (Rou Cong Rong) 15 g, Angelicae sinensis Radix (Dang Gui) 12 g, Salviae miltiorrhizae Radix (Dan Shen) 12 g, Cyperi Rhizoma (Xiang Fu) 12 g. During the luteal phase, we modified the formula and added Lycii Cortex (Di Gu Pi)15 g, Anemarrhenae Rhizoma (Zhi Mu) 12 g, Phellodendri Cortex (Huang Bai) 12 g. During the late follicular phase and ovulation phase, we added Epimedii Herba (Xian Ling Pi) 12 g, Curculiginis Rhizoma (Xian Mao)12 g, and Leonuri Fructus (Chong Wei Zi) 12 g.
To prepare for the decoction, the patient was instructed to add 600 mL of water to the raw herbs, bring the water-herbs-mixture to a boil, turn back down to a light rolling boil for 25 min, and then strain the liquid from the mixture to drink. The patient was asked to decoct the herbs and drink them twice daily. After three months of the Chinese herbal medicine treatment alone, the patient had two chemical preg- nancies in December 2015 (Fig. 2A) and in January 2016 (Fig. 2B). Due to emotional frustration and psychological stress from two disappointed chemical pregnancies, the patient decided to take a break from fertility treatments and temporarily stopped taking the herbal formula for four months, from April to June 2016. After stopping the herbal treatment, the patient discovered that her menstrual cycle turned short again, so she decided to resume taking the herbal formula. After going back to treatment for another two months, the patient had a positive urine
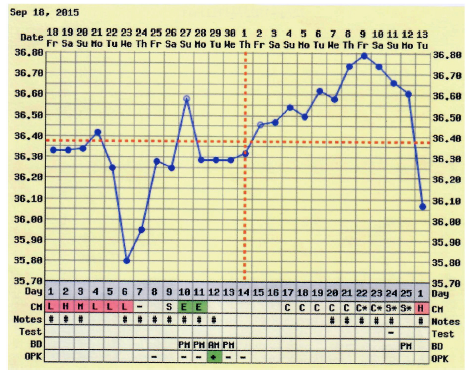
Fig. 1. At the beginning of Chinese herbal medicine (CHM) treatment, the patient’s basal body temperature (BBT) showed a short menstrual cycle, a slow rise of temperature after ovulation, and inconsistent shifts in the luteal phase.
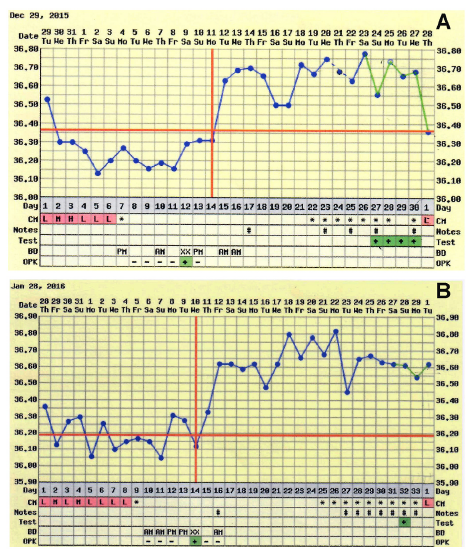
Fig. 2. After CHM treatment, the patient had two positive pregnancies, though basal body temperature showed chemical pregnancies. A: the first chemical pregnancy was in December 2015; B: the second chemical pregnancy was in January 2016.
pregnancy test on August 24, 2016 (Fig. 3), and her LMP was on August 2, 2016. On May 1, 2017, she gave birth to a healthy baby boy.
On Jun 20, 2020, the patient returned to our clinic at the age of 47. Her chief complaint was that she and her husband had been trying to conceive a second child for about two years without success. She had short menstrual cycles of 22–27 days, a moderate quantity of menses, and no menstrual cramps. On her return visit, her LMP was on June 11, 2020, and her BBT showed a short luteal phase (Fig. 4). Laboratory blood test was performed on menstrual cycle day 2 (November 19, 2020): FSH: 27.1 mIU/mL (Postmenopausal: 23–116.3mIU/mL); LH: 5.2
mIU/mL (follicular phase: 1.9–12.5); FSH/LH > 5; AMH: 0.07 ng/mL (>49yrs < 0.45). After taking “Fu Kun Tang” decoction with modifica-
tions for five months, the patient had a positive urine pregnancy test on December 10, 2020 (Fig. 5), and her LMP was on November 18, 2020. In addition, her blood test for Human Chorionic Gonadotropin (hCG) value was at 431mIU/mL (>5 mIU/mL pregnancy) on December 15, 2020. Her noninvasive prenatal testing (NIPT) result showed a low risk for
microdeletions aneuploidies, and the fetal sex was determined to be male on January 27, 2021. The patient gave birth to another healthy boy on August 20, 2021.
3.Discussion
Age-related infertility is often considered a problem that can be easily solved by the application of ART. However, it is well established that maternal age is associated with a rapid decline in the production of healthy and high-quality oocytes resulting in reduced fertility in women older than 35 years of age, even with ART treatment. Despite the pro- found changes in numbers and quality of follicles, the process of ovarian aging remains largely unnoticed. The events that can be quite easily recognized are cycle irregularity, with the first subtle clinical sign of advancement in the reproductive aging process is a shortening of the
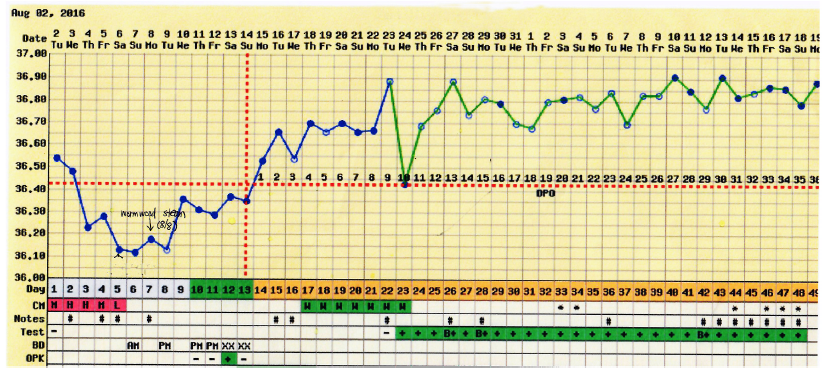
Fig. 3. After CHM treatment, the patient had a positive urine pregnancy test on August 23, 2016, which resulted in a healthy live birth on May 1, 2017.
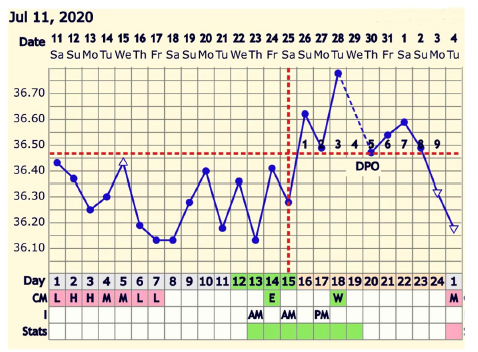
Fig. 4. On June 20, 2020, the patient returned to treatment at age 47 after two years of trying to conceive a second child without success. Before CHM treat- ment, the patient’s BBT showed a short menstrual cycle and luteal phase deficiency.
length of the menstrual cycle by 2–3 days [9], shortened follicular phase with elevated FSH [10], and FSH rise occurring earlier during the luteal phase [11]. This suggests that dominant follicle growth starts earlier, even before the onset of menses, with higher levels of estradiol present in the subsequent early follicular phase. The main reasons for age-related infertility include reduced ovarian reserve and decreased oocyte/embryo competence due to aging insults, especially concerning an increased incidence of aneuploidies, and possibly decreased mito- chondrial activity [12].
The patient here had severe diminished ovarian reserve, which was indicated by her laboratory test results. When the patient was trying to conceive in 2015, her baseline value of FSH was above 26. In 2020, her baseline FSH was 27.10, and AMH was 0.07. She also had short men- strual cycle lengths. AMH hormone is a reliable marker for assessing the age-related decline of the ovarian reserve in healthy women. Moreover, the aging effect on live birth rates was more strongly mediated by AMH and less by FSH [13]. The threshold value for low ovarian reserve is defined by an AMH level of 0.7 ng/mL [14]. The patient’s hormone levels suggested a perimenopausal status and indicated a severe
diminished ovarian follicular pool. Low AMH is independently associ- ated with lower live birth and higher IVF cycle cancellation rates [15], therefore most IVF clinics set 45 years of age as an upper age limit for allowing IVF treatment using patients’ own eggs [16].
With the loss of ovarian follicular pool and short menstrual cycles, are any herbal remedies that can help adjust the length of the menstrual cycle back to normal? Fu Qing-zhu, a TCM gynecologist in the Qing dynasty (1607–1684), offered his expertise on this topic. In his book “Fu Qing-zhu Gynecology”, he dedicated a special chapter to discuss the condition of short menstrual cycles and contributed two classical herbal formulas [17]. Since then, both herbal formulas have been widely used by TCM practitioners.
3.1. Taiji Yin-Yang and menstrual regulation
The concept of Yin and Yang serves as the foundation for under- standing health, as well as diagnosing and treating illness. TCM believes that Yin and Yang maintain a dynamic balance during the entire men- strual cycle. According to ancient literature, we have been using the Taiji Yin-Yang diagram to illustrate the dynamic balance in the men- strual cycle (Fig. 6). The primordial eight trigrams (Ba Gua) originated in China. Each trigram consists of three lines. In the cycle of Taiji Yin- Yang diagram, the “broken” line (- -) and black-colored part represent
Yin, and the “unbroken” line (-) and white-colored part represent Yang.
Yin and Yang are opposite and interdependent. They mutually consume each other and inter-transform into each other. The dynamic relation- ship creates movements to maintain the homeostasis of Yin and Yang in a monthly Taiji cycle. A synchronous relationship between menstrual cycles and lunar rhythms has been illustrated by previous studies [18–20].
Tang Rongchuan (1846–1897) from the Qing dynasty believed that the full moon represents the pure Yang, and the new moon represents the pure Yin. During the follicular phase, Yin generates Yang, and Yang will reach its peak until ovulation. Yang symbolizes dominance, crea- tivity, strength, warmth, movement, activity, upgrade, and positive feedback. During the luteal phase, Yang generates Yin, and Yin will reach its peak until menstruation. Yin symbolizes compliance, obedi- ence, smoothness, peace, sequence, downgrade, and negative feedback. The Yin-Yang theory corresponds with the modern reproductive health principle. The Yang phase (preovulation to mid-luteal phase) manifests as higher levels of sex hormones and LH positive feedback to estrogen, resulting in more LH and more upstream estrogen release. On the other hand, the Yin phase (late luteal phase to early follicular phase) manifests as lower levels of sex hormones and progesterone negative feedback to
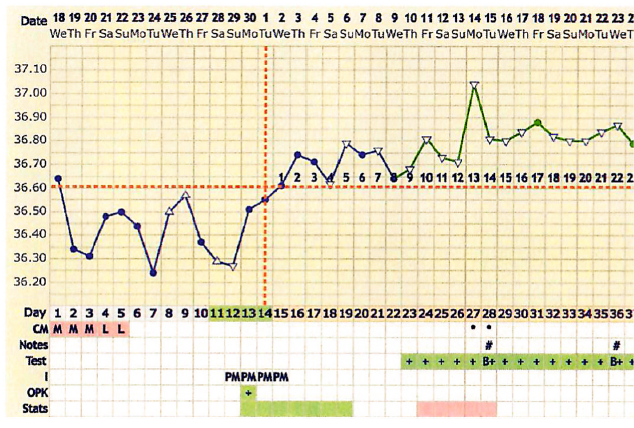
Fig. 5. After CHM treatment, the patient had a positive urine pregnancy test on December 10, 2020. She gave birth to a healthy boy on August 20, 2021.
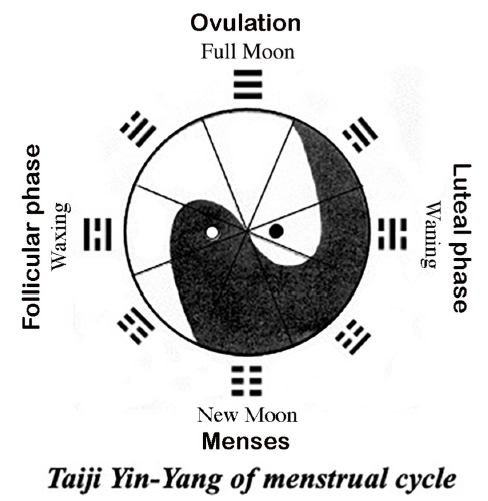
Fig. 6. Illustration of Taiji Yin-Yang of the menstrual cycle. “broken” line (- -) and black-colored part represent Yin, “unbroken” line (-) and white-colored part represent Yang. During the follicular phase, Yin generates Yang, Yang
will gradually reach its peak until ovulation. During the luteal phase, Yang generates Yin, Yin will gradually reach its peak until menstruation.
GnRH and LH, where increased progesterone levels decrease the up- stream release of GnRH and LH [21,22]. Therefore, the Yin-Yang theory provided a framework not just for Chinese philosophy but also for the fields of biology and medicine [23].
3.2. Treatment rationale according to TCM theory
According to the Yin-Yang principle, we prescribed a herbal formula named “Fu Kun Tang” to stimulate ovulation and promote regular
menstruation. Clinical trials and animal experiments demonstrated that “Fu Kun Tang” can significantly promote the ovarian development of pubertal mice aged 26–30 days (P < 0.05) (Fig. 7 A and B) [24]. To treat
short menstrual cycles, we add Yin-nourishing herbs during the luteal
phase, such as Lycii Cortex, Anemarrhenae Rhizoma, and Phellodendri Cortex, to control FSH levels to prevent the antral follicular growth in the early luteal phase. During the later follicular and ovulation phase, we add Yang-tonifying herbs, such as Epimedii Herba, Curculiginis Rhizoma, and Leonuri Fructus, to improve the follicular quality and elevate the LH peak during ovulation. Modern pharmacological exper- iments have shown that the main active ingredients of Epimedii Herba include total flavonoids of epimedium (TFE) and icariin (ICA). In a previous animal study, icariin was shown to improve the ovarian endocrine function in rat ovarian granulosa cell culture in vitro by pro- moting the secretion of estradiol and progesterone through up-regulation of CYP19 and CYP19 [25]. In vivo study (rat model) showed that icariin administration elevated the serum levels of female hormone estradiol (E2), testosterone (T), and interleukin (IL)-2, decreased levels of FSH and LH, and promoted the expression levels of estrogen receptor (ER) and ERα in the hypothalamus [26]. Given the previous pharmacological studies, we hypothesize that some Yang-tonifying herbs can increase hormone receptor sensitivity. Since Yang reaches its peak during the ovulation phase, we added Leonuri Fructus and Salviae miltiorrhizae Radix to enhance the blood circulation of the ovary to further activate Yang. Our previous molecular study has demonstrated that the plasminogen activator system is also involved in the process of ovulation [27]. Therefore, adding blood-moving herbs during the ovulation phase can promote ovulation. Further molecular experiments and pharmaceutics studies are needed to uncover the exact mechanism involved.
3.3. BBT is a valuable utilized method
BBT measurements have been used for decades to help women optimize the timing of intercourse during a fertile window [28]. Although, studies have expressed the viewpoint that BBT is an unreliable technique to determine accurate ovulation timing but would be of use if the clinical precision required for the diagnosis of ovulation were less [29], and revealed underrecognized age-dependent changes in men- strual cycle length and BBT, which will contribute to a better under- standing of female reproductive health [30]. The amplitude of the
Fig. 7. H&E staining was performed on the vertical sections of the mice ovaries (X100). Oral administration of “Fu Kun Tang” extracts were given at 0.3mL/10 g body weight for seven days. A typical pubertal mice of 26–30 days weighed 17–19 g. In the control group (A), mice were treated with sterilized water. In treatment group (B), mice were treated with “Fu Kun Tang” extract. Histopathology report showed that the treatment group had a significant amount more mature follicles than the control group. n = 15/group, P < 0.05 (T-test).
temperature rise was independent of the concentration of progesterone and the type of hormonal stimulation [31]. Whilst LH test kits have been used to determine the day of ovulation for decades, they also have a significant margin of error when used in isolation. The addition of using BBT and fertility apps may help further narrow down the ovulation fertile window. Moreover, BBT provides valuable data for retrospective analysis of ovulation function, luteal function, chemical pregnancy, luteinizing unruptured follicle syndrome (LUFs), and evaluation of treatment efficacy.
Therefore, BBT is a valuable, low-cost, and user-friendly tool to track hormonal changes, predict and review a more accurate ovulation win- dow. Especially, the length of the luteal phase can provide an insight into a person’s fecundability and increase the chances of detecting subfertility early.
4.Conclusions
In this case study, we discussed a patient of advanced maternal age with severe diminished ovarian reserve who was able to conceive naturally twice and give birth to two boys at age 43 and age 47 after the treatment of Chinese herbal medicine. The patient was diagnosed with secondary infertility, severe diminished ovarian reserve, and a short menstrual cycle. Here, we used “Fu Kun Tang” with modifications to improve ovulation function and promote regular menstruation based on Yin-Yang principles and BBT’s feedback. This case demonstrated how Chinese herbal medicine can benefit a patient with advanced maternal age by improving her ovarian function and oocyte quality. We need more evidence from pharmacokinetic studies, in vitro and in vivo animal studies, and clinical trials to further identify the mechanism of action and support the effectiveness of traditional Chinese herbs in improving fecundity rates.
Funding
No external funding was received for this case report.
Consent
Author obtained informed consent from the patient for publication of this case report.
CRediT authorship contribution statement Xiaoxiong Shen: Writing – original draft.
Declaration of competing interest
The author declares that there is no conflict of interest.
References
[1] M. Mikwar, A.J. MacFarlane, F. Marchetti, Mechanisms of oocyte aneuploidy associated with advanced maternal age, Mutat. Res. Rev. Mutat. Res. 785 (2020) 108320. Jul-Sep.
[2] A.M. Fernandez, P. Drakopoulos, J. Rosetti, V. Uvin, S. Mackens, et al., IVF in women aged 43 years and older: a 20-year experience, Reprod. Biomed. Online 42
(4) (2021) 768–773.
[3] H. Hipp, S. Crawford, J.F. Kawwass, S.L. Boulet, D.A. Grainger, et al., National trends and outcomes of autologous in vitro fertilization cycles among women ages 40 years and older. J Assist Reprod Genet 34 (7) (2017) 885–894.
[4] F.M. Ubaldi, D. Cimadomo, A. Vaiarelli, G. Fabozzi, R. Venturella, et al., Advanced maternal age in IVF: still a challenge? The present and the future of its treatment, Front. Endocrinol. 10 (2019) 94. Feb;20.
[5] E. Somigliana, A. Paffoni, A. Busnelli, F. Filippi, L. Pagliardini, Age-related infertility and unexplained infertility: an intricate clinical dilemma, Hum. Reprod. 31 (7) (2016) 1390–1396.
[6] X. Shen, S. Bagherigaleh, Acupuncture and pregnancy: classical meets modern, Med. Acupunct. 31 (5) (2019) 248–250, 1.
[7] K. Ried, K. Stuart, Efficacy of Traditional Chinese Herbal Medicine in the management of female infertility: a systematic review, Compl. Ther. Med. 19 (6) (2011) 319–331.
[8] J.W. Lee, M.K. Hyun, H.J. Kim, D.I. Kim, Acupuncture and herbal medicine for female infertility: an overview of systematic reviews, Integr Med Res 10 (3) (2021) 100694.
[9] F.J. Broekmans, M.R. Soules, B.C. Fauser, Ovarian aging: mechanisms and clinical consequences, Endocr. Rev. 30 (5) (2009) 465–493.
[10] F. Miro, L.J. Aspinall, The onset of the initial rise in follicle-stimulating hormone during the human menstrual cycle, Hum. Reprod. 20 (1) (2005) 96–100.
[11] P. van Zonneveld, G.J. Scheffer, F.J. Broekmans, M.A. Blankenstein, F.H. de Jong, et al., Do cycle disturbances explain the age-related decline of female fertility? Cycle characteristics of women aged over 40 years compared with a reference population of young women, Hum. Reprod. 18 (3) (2003) 495–501.
[12] D. Cimadomo, G. Fabozzi, A. Vaiarelli, N. Ubaldi, F.M. Ubaldi, et al., Impact of maternal age on oocyte and embryo competence, Front. Endocrinol. 29 (9) (2018) 327.
[13] B. Meczekalski, A. Czyzyk, M. Kunicki, A. Podfigurna-Stopa, L. Plociennik, et al., Fertility in women of late reproductive age: the role of serum anti-Müllerian hormone (AMH) levels in its assessment, J. Endocrinol. Invest. 39 (11) (2016) 1259–1265.
[14] A.Z. Steiner, A.H. Herring, J.S. Kesner, J.W. Meadows, F.Z. Stanczyk, et al., Antimüllerian hormone as a predictor of natural fecundability in women aged 30- 42 years, Obstet. Gynecol. 117 (2011) 798–804.
[15] S. Ligon, M. Lustik, G. Levy, B. Pier, Low antimüllerian hormone (AMH) is associated with decreased live birth after in vitro fertilization when follicle- stimulating hormone and AMH are discordant, Fertil. Steril. 112 (1) (2019) 73–81.
[16] F.M. Ubaldi, D. Cimadomo, A. Capalbo, A. Vaiarelli, L. Buffo, et al., Preimplantation genetic diagnosis for aneuploidy testing in women older than 44 years: a multicenter experience, Fertil. Steril. 107 (5) (2017) 1173–1180.
[17] Translated by Yang Shou-Zhong Liu Da-Wei. Fu Qing-Zhu’s Gynecology, Blue poppy press Inc, 2002.
[18] S.P. Law, The regulation of menstrual cycle and its relationship to the moon, Acta Obstet. Gynecol. Scand. 65 (1) (1986) 45–48.
[19] S. Luo, Y. Luo, Preliminary study on the relationship between menstrual rhythm and lunar phase, Shanghai J TCM (12) (1984) 42–44 (Chinese).
[20] C. Helfrich-Fo¨rster, S. Monecke, I. Spiousas, T. Hovestadt, O. Mitesser, T.A. Wehr, Women temporarily synchronize their menstrual cycles with the luminance and gravimetric cycles of the Moon, Sci. Adv. 27 (5) (2021) eabe1358, 7.
[21] N. Simi´c, A. Ravli´c, Changes in basal body temperature and simple reaction times during the menstrual cycle, Arh. Hig. Rada. Toksikol. 64 (1) (2018) 99–106.
[22] E. Terasawa, Neuroestradiol in regulation of GnRH release, Horm. Behav. 104
